Exploring the Effect of Ammonia on Murine Mesenteric Microvasculature
Introduction
Patients with cirrhosis often have low blood pressures due to systematic vasodilation that puts them at risk for progressive renal failure, Hepatorenal syndrome (HRS). Clinically, the exact mechanisms underlying the systemic vasodilation is not known. Ammonia has been shown to dilate the basilar artery of rabbits via its directs effects on vascular smooth muscle cells. However, the effect of ammonia on the vasculature and blood pressures is still unknown. The purpose of our study was to investigate whether ammonia has a role in causing vasodilation of the microvasculature.
Methods
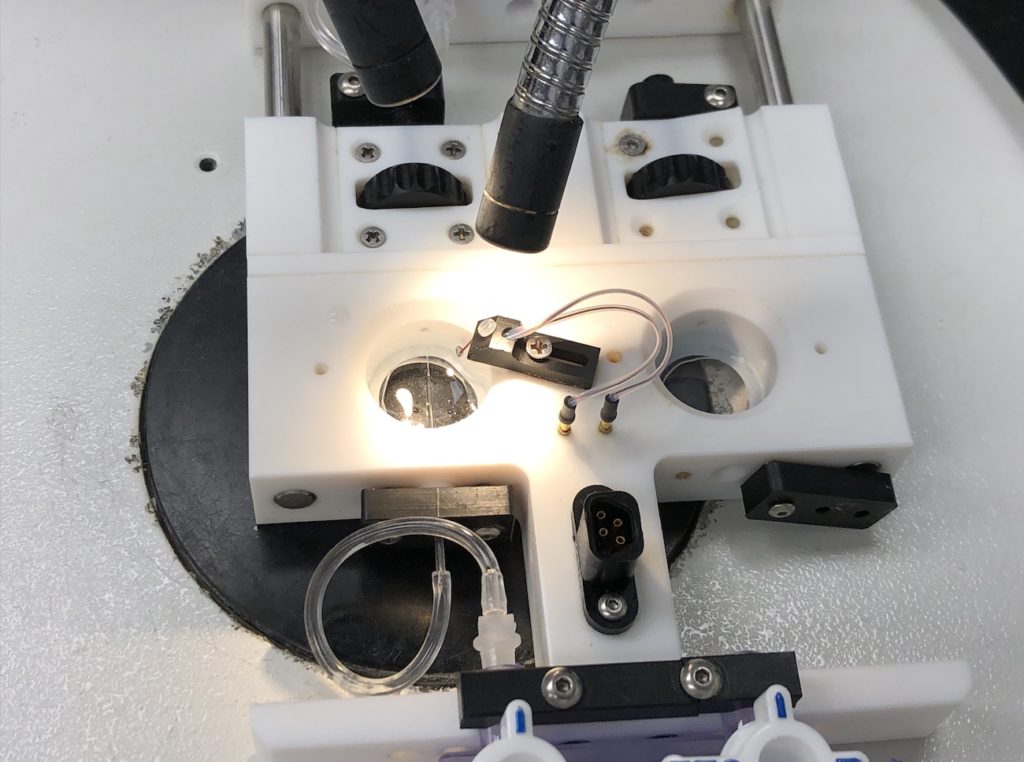
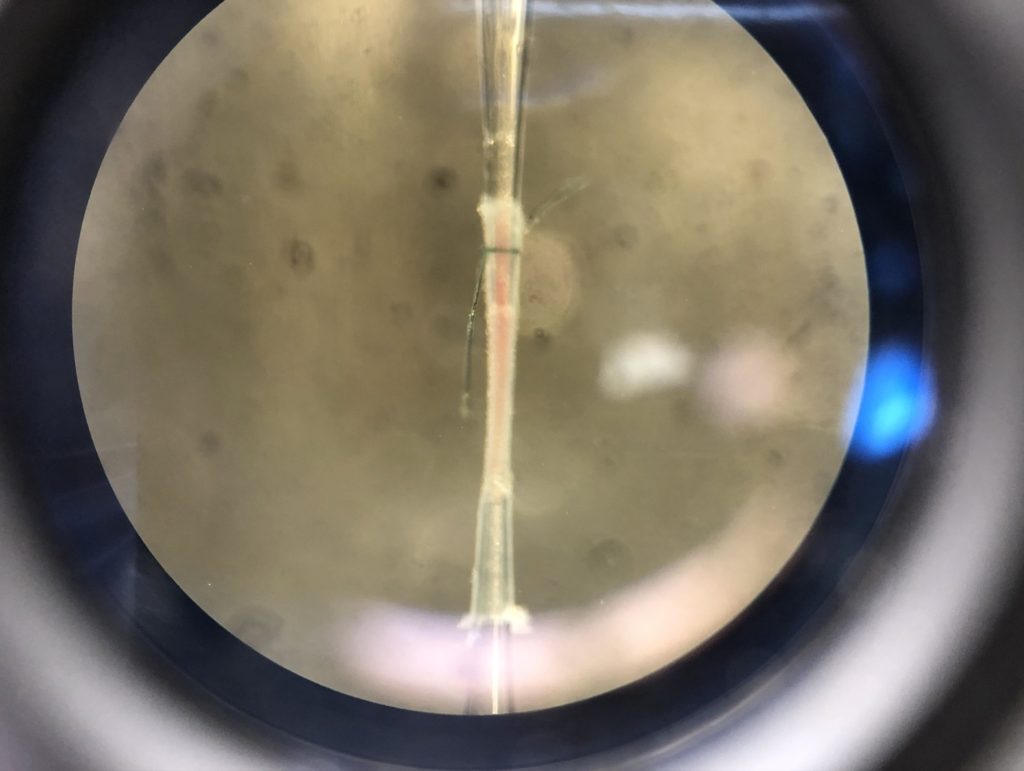
We carefully dissected the mesenteric blood vessels from adult male mice. Then we would hang and tie the second-order mesenteric arteries (about 150- 200 µm in diameter) onto two cannulas and test if it holds pressure. If it does, we then would equilibrate the vessel with warm buffer at 37 degree Celsius and 60 mmHg for 20 minutes. After that we added increasing doses of phenylephrine to constrict the vessel to 50% of initial diameter. We then investigated whether addition of increasing doses of ammonia increased the luminal diameter. We then assessed the effect of ammonia in the presence of an inhibitor of inducible nitric oxide synthase (iNOS) to determine if the effects were dependent on the endothelium or independent.

Results
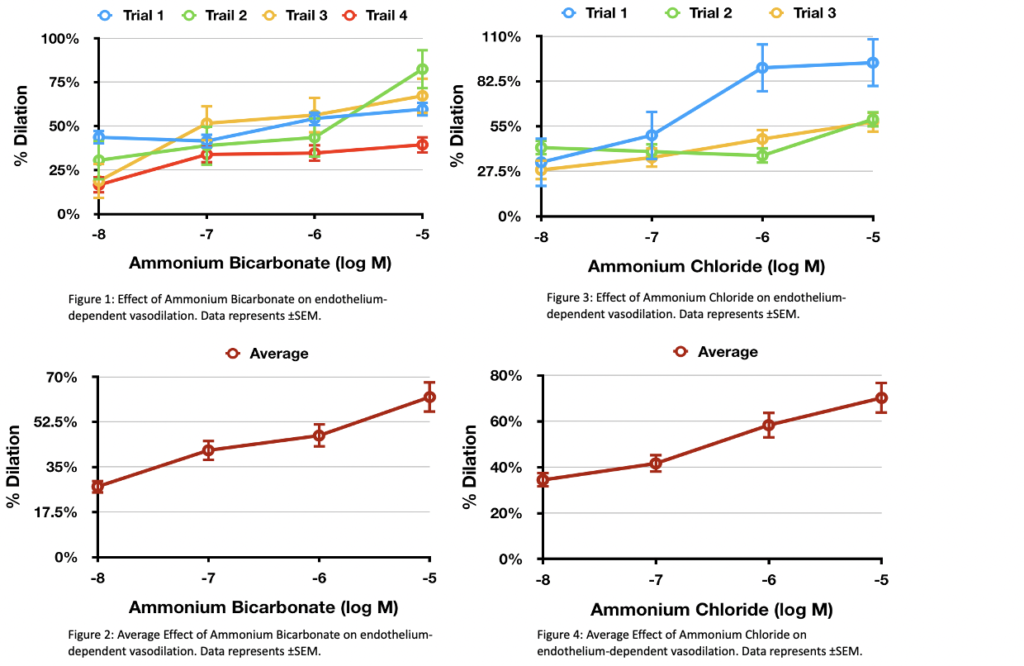
Our preliminary data shows ammonia is a vasodilator at doses ranging from 10^-8M to 10^-5M. The maximal dilation was 44.32%. Figure 1 and 3 demonstrate all trials from ammonium bicarbonate and ammonium chloride. Although there are variations within the data, there is an overall upward trend. Figure 2 and 4 are the averages of all the data points, showing an upward trend indicating ammonia does have a vasodilatory effect.
Future Directions
In the future, we will use an iNOS inhibitor to discern whether the effect of ammonia is dependent on the endothelium. We will also do further in vitro studies to find the molecular signaling pathways mediating these effects. There are currently no effective treatment options for patients with liver disease and renal failure. If our hypothesis is true, there could be a potential therapeutic target for an otherwise almost uniformly fatal disease.